The Perineum
The perineum is an anatomical region in the pelvis. It is located between the thighs and represents the most inferior part of the pelvic outlet. The perineum is separated from the pelvic cavity superiorly by the pelvic floor.
This region contains structures that support the urogenital and gastrointestinal systems – and it, therefore, plays an important role in functions as such micturition, defecation, sexual intercourse, and childbirth.
In this article, we shall look at the anatomy of the perineum – its boundaries, contents, and clinical correlations.

Fig 1 – The perineum is located between the thighs.
Boundaries
In clinical practice, the term “perineum” is frequently used to describe the area between the external genitalia and the anus. However, in anatomical terms, the perineum is a diamond-shaped structure.
There are two main ways in which the boundaries of the perineum can be described. The anatomical borders refer to its exact bony margins, whilst the surface borders describe the surface anatomy of the perineum.
Anatomical Borders
The anatomical borders of the perineum are:
- Anterior – pubic symphysis.
- Posterior – the tip of the coccyx.
- Laterally – inferior pubic rami and inferior ischial rami, and the sacrotuberous ligament.
- Roof – the pelvic floor.
- Base – skin, and fascia.
The perineum can be subdivided by a theoretical line drawn transversely between the ischial tuberosities. This split forms the anterior urogenital triangle and the posterior anal triangle. These triangles are associated with different components of the perineum.
Surface Borders
The surface boundaries are best shown when the lower limbs are abducted, and a diamond shape is depicted:
- Anterior – mons pubis in females, the base of the penis in males.
- Laterally – medial surfaces of the thighs.
- The posterior–superior end of the intergluteal cleft.
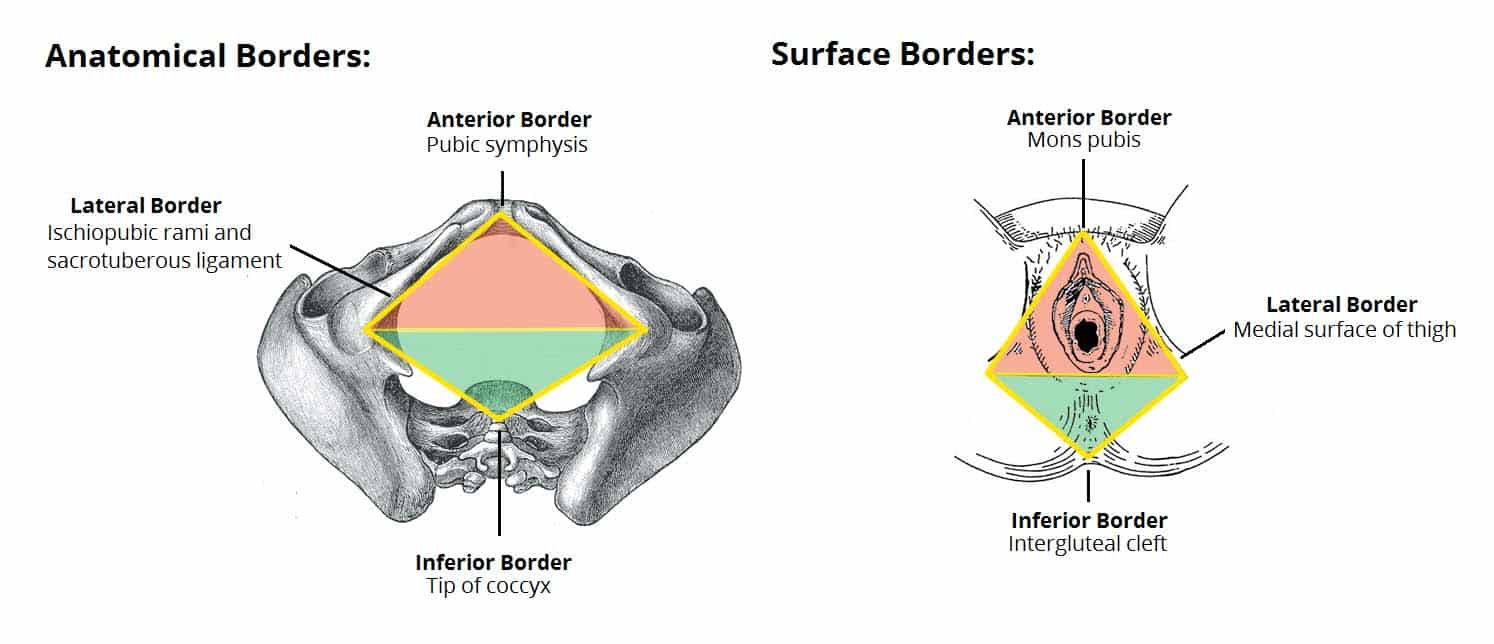
Fig 2 – Anatomical and surface borders of the perineum.
Contents
The perineum can be subdivided by a theoretical line drawn transversely between the ischial tuberosities. This split forms the anterior urogenital and posterior anal triangles.
These triangles are associated with different components of the perineum – which we shall now examine in more detail.
Anal Triangle
The anal triangle is the posterior half of the perineum. It is bounded by the coccyx, sacrotuberous ligaments, and a theoretical line between the ischial tuberosities.
The main contents of the anal triangle are:
- Anal aperture – the opening of the anus.
- External anal sphincter muscle – voluntary muscle responsible for opening and closing the anus.
- Ischioanal fossae (x2) – spaces located laterally to the anus.
The anal aperture is located centrally in the triangle with the ischioanal fossae on either side. These fossae contain fat and connective tissue, which allow for the expansion of the anal canal during defecation. They extend from the skin of the anal region (inferiorly) to the pelvic diaphragm (superiorly).
Another important anatomical structure within the anal triangle is the pudendal nerve, which supplies the whole perineum with somatic fibers.
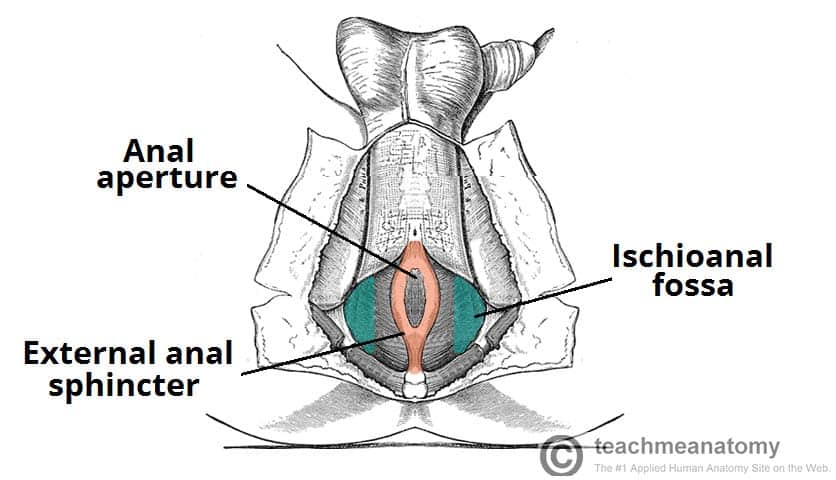
Fig 3 – Contents of the anal triangle.
Urogenital Triangle
The urogenital triangle is the anterior half of the perineum. It is bounded by the pubic symphysis, ischiopubic rami, and a theoretical line between the two ischial tuberosities. The triangle is associated with the structures of the urogenital system – the external genitalia and urethra.
Structurally, the urogenital triangle is complex, with a number of fascial layers and pouches. Unlike the anal triangle, the urogenital triangle has an additional layer of strong deep fascia; the perineal membrane. This membrane has pouches on its superior and inferior surfaces.
The layers of the urogenital triangle (deep to superficial):
- Deep perineal pouch – a potential space between the deep fascia of the pelvic floor (superiorly) and the perineal membrane (inferiorly). It contains part of the urethra, external urethral sphincter, and the vagina in the female. In males, it also contains the bulbourethral glands and the deep transverse perineal muscles.
- Perineal membrane – a layer of tough fascia, which is perforated by the urethra (and the vagina in the female). The role of the membrane is to provide attachment for the muscles of the external genitalia.
- Superficial perineal pouch – a potential space between the perineal membrane (superiorly) and the superficial perineal fascia (inferiorly). It contains the erectile tissues that form the penis and clitoris, and three muscles – the ischiocavernosus, bulbospongiosus, and superficial transverse perineal muscles. The greater vestibular glands (Bartholin’s glands) are also located in the superficial perineal pouch. The pouch is bounded posteriorly to the perineal body.
- Perineal fascia – a continuity of the abdominal fascia that has two components:
- Deep fascia: covers the superficial perineal muscles and protruding structures (e.g. penis & clitoris).
- Superficial fascia is composed of further two layers fascia:
- Superficial layer – continuous with Camper’s fascia of the anterior abdominal wall
- Deep layer (Colles’ fascia) – continuous with Scarpa’s fascia of the anterior abdominal wall
- Skin – The urethral and vaginal orifices open out onto the skin.
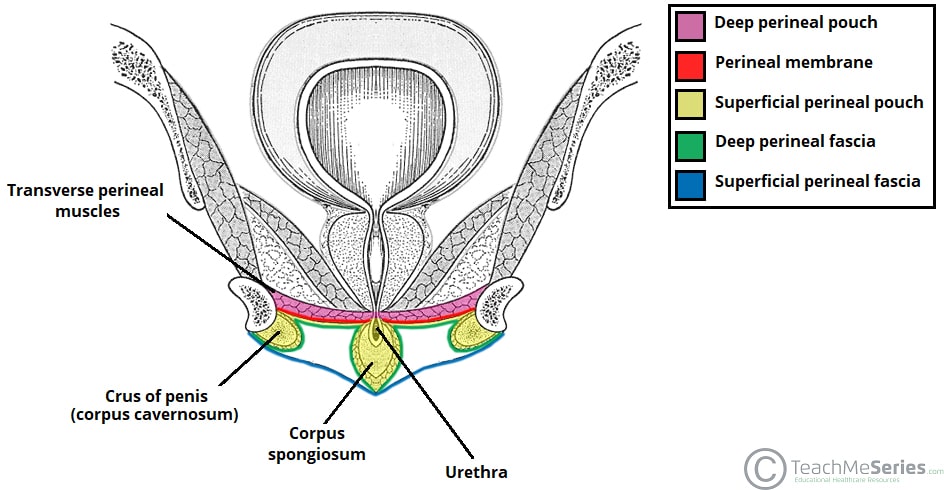
Fig 4 – Coronal section of the male pelvis, showing the layers of the urogenital triangle.
The Perineal Body
The perineal body is an irregular fibromuscular mass. It is located at the junction of the urogenital and anal triangles – the central point of the perineum. This structure contains skeletal muscle, smooth muscle, and collagenous and elastic fibers.
Anatomically, the perineal body lies just deep into the skin. It acts as a point of attachment for muscle fibers from the pelvic floor and the perineum itself:
- Levator ani (part of the pelvic floor).
- Bulbospongiosus muscle.
- Superficial and deep transverse perineal muscles.
- External anal sphincter muscle.
- External urethral sphincter muscle fibers.
In women, it acts as a tear-resistant body between the vagina and the external anal sphincter, supporting the posterior part of the vaginal wall against prolapse. In the male, it lies between the bulb of the penis and the anus.
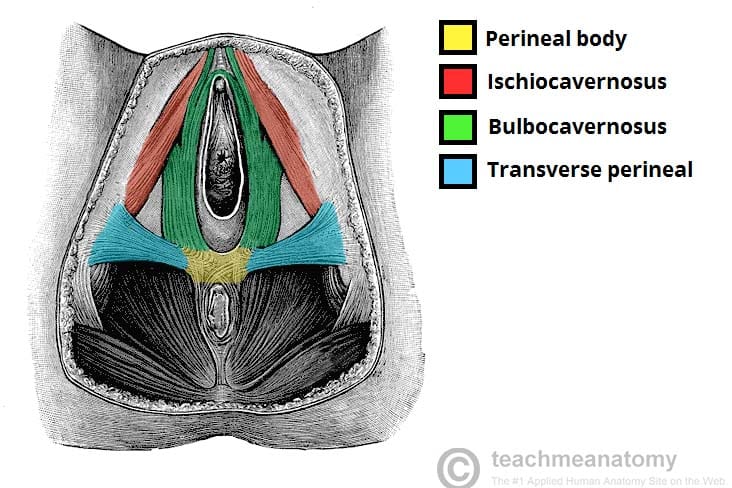
Fig 5 – Muscles attaching to the perineal body.
Neurovascular Supply
The major neurovascular supply to the perineum is from the pudendal nerve (S2 to S4) and the internal pudendal artery.
The pudendal nerve (along with the internal pudendal artery and vein) travels along the inner surface of the ischial tuberosities, through a “canal” formed by a thickening of the obturator fascia (Alcock’s canal). The pudendal neurovascular bundle courses downwards through each ischioanal fossa and gives branches to both the anal and genital triangles.
Clinical Relevance – The Perineal Body
The perineal body is a central attachment for perineal muscles, and functions to support the pelvic floor.
Childbirth can lead to damage (stretching/tearing) of the perineal body, thus leading to possible prolapse of pelvic viscera. This may be avoided by an episiotomy (a surgical cut in the perineum). This inevitably causes damage to the vaginal mucosa but prevents uncontrolled tearing of the perineal body.
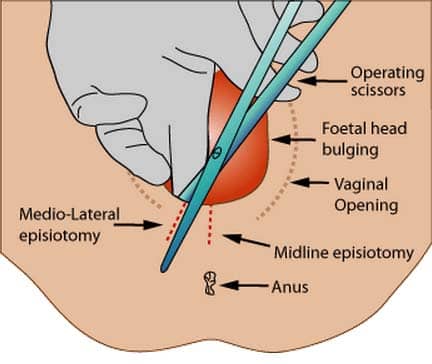
Fig 6 – An episiotomy is delivered to avoid tearing of the perineum and/or the pelvic floor. There are two different episiotomies that can be performed.
Clinical Relevance – Bartholin’s Gland Cysts
The Bartholin’s glands are located within the superficial perineal pouch of the urogenital triangle. Their role is to make a small amount of mucus-like fluid.
Normally, Bartholin’s glands are not detected on physical examination. However, if the duct becomes blocked, then these glands can swell to form fluid-filled cysts.
These cysts can become infected and inflamed, a condition known as bartholinitis. The most common cause of infection is from bacteria such as Staphylococcus spp. and Escherichia coli.
The article was originally published here.


Comments are closed.