Foot Eczema
Eczema On Feet: Foot eczema causes the skin on the foot to become red, itchy, and inflamed. Eczema, also known as dermatitis, is a common condition, particularly in childhood. It affects approximately 10-20% of children, and whilst a majority grow out of it by the age of ten, 3% of adults go on to suffer from eczema periodically.
Eczema can affect any part of the foot but most typically develops on the toes, heel, sides, and ball of the foot.
Foot eczema usually develops in response to friction, moisture, or an allergic reaction.
While there is no specific cure for foot eczema, treatment aims to reduce itching and inflammation and to help the skin to retain moisture.
Common Types Of Foot Eczema
There are a number of different types of foot eczema, the most common being atopic dermatitis. Here we will look at the most common types of foot eczema, what causes them, and the symptoms associated with them and then we will go on to look at the best ways to treat eczema.
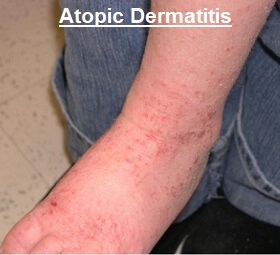
1. Atopic Dermatitis
Atopic dermatitis is the most common type of foot eczema. It is a chronic condition, which means it is long-lasting.
Symptoms of atopic dermatitis often come and go with periods of “flare-ups”. It typically starts during childhood (before the age of two) and in some cases persists through teenage years and into adulthood.
Symptoms Of Atopic Dermatitis
Foot eczema from atopic dermatitis usually presents with the following symptoms:
-
- Skin Changes: the skin becomes dry and scaly and may even thicken and crack
- Itching: Atopic eczema is almost always itchy, and this itchiness may develop before there are any other signs of foot eczema, such as a rash or any redness.
-
- The itchiness often gets worse at night
-
- Redness: Patches of red skin develop, most typically around the toes, underneath the foot, and on the heel
- Soreness: The skin often becomes very sensitive and sore, especially if you have been scratching a lot due to the itchiness
- Flare-Ups: Symptoms of atopic dermatitis tend to come and go. People often go through periods of several weeks/months with no symptoms, only for the itching and redness to come back, typically in the same place
- Infection: Repeated scratching can damage the skin and lead to an infection. The most common type of infection with eczema is Staph A. Sores may develop that “weep” or they may form a yellow crust or small bumps filled with pus
Eczema may be quite widespread affecting not just the foot but other areas too, most commonly the back of the knees, hands, front of the elbows, and the head.
What Triggers Atopic Dermatitis?
The exact cause of foot eczema from atopic dermatitis is unknown. It is thought to be caused by the immune system overreacting to certain allergens or irritants, either inside or outside the body, which causes inflammation.
People with eczema find that their skin is unable to retain moisture so the skin becomes dry which increases the likelihood of reactions to certain triggers. There may be a lack of filaggrin in the skin, a protein that maintains a healthy, protective skin barrier that stops moisture from escaping and this makes it easier for viruses and bacteria to enter the skin. Studies have shown that nearly 50% of all cases of severe eczema have at least one mutated filaggrin gene.
Atopic dermatitis is also more likely if you suffer from hay fever and/or asthma. These three allergic conditions are collectively known as the “atopic triad” and are often present together.
There is also a suspected genetic link with an increased chance of developing foot eczema and atopic dermatitis if you have family members with any of the atopic triads.
It is important to remember that atopic dermatitis is not contagious, you can’t pass it on to anyone else.
2. Dyshidrotic Eczema

Also known as Dishydrosis or Pompholyx, dyshidrotic foot eczema causes tiny, deep blisters to develop on the soles and sides of the feet and the palms of your hand.
When it affects just the feet it is called Pedopompholyx.
The first sign of dyshidrotic eczema is intense itching of the soles of the feet, sides of the toes, and fingers and it may feel like the skin is burning.
Tiny blisters then develop which may be filled with fluid. The skin may become infected, especially if you are scratching lots, making the blisters extremely painful and they may start to ooze out pus. In severe cases, large blisters will form.
The blisters from dyshidrotic eczema usually clear up after a few weeks – the skin typically dries and cracks as it is healing.
Dyshidrotic eczema is thought to be caused by a fungal infection, a reaction to an allergen such as metals or soaps, stress, seasonal allergies, and sweating. It usually affects adults between the ages of 20-40 and is thought to be hereditary.
3. Nummular Eczema

Also known as Nummular Dermatitis or Discoid Eczema, this causes patches of coin-shaped spots to develop which may ooze or crust over. The skin around the lesions turns red or brown and becomes inflamed. The spots may or may not be itchy.
Nummular eczema may develop in response to skin damage such as a burn or insect bite, inflammation elsewhere in the body, dry skin, poor blood flow, or as a reaction to certain metals.
There does not appear to be any hereditary link with nummular eczema unlike with other types of foot eczema. 1It also tends not to be recurring and usually clears up completely within a year. It usually affects men between the ages of 55-65 and women aged 13-25. It can also affect children.
4. Contact Dermatitis

There are two types of contact dermatitis.
Allergic Contact Dermatitis: caused by an immune response to an irritant such as metal or latex, and
Irritant Contact Dermatitis: This develops when your skin is irritated by a chemical or similar substance.
Symptoms of contact dermatitis usually develop very quickly after exposure to the irritant with the skin turning red and itchy and blisters forming which may be filled with pus. You can find out more about both types of contact dermatitis in the foot rash section.
Common Causes Of Foot Eczema
Foot eczema may be triggered and made worse by:

- Irritants: Such as soaps & detergents e.g. washing powder/liquid, shampoo, body wash, bubble bath, and washing up liquid
- Stress: Eczema flare-ups are often triggered by periods of stress
- Weather: Cold, dry weather, damp, or very hot weather can increase itching
- Hormones: women often find their eczema gets worse during pregnancy or just before their monthly period
- Food Allergies: common allergies linked with atopic dermatitis include cow’s milk, peanuts, wheat, and eggs
- Other Allergens: from everyday materials such as dust mites, seasonal pollen, and pet dander (tiny scales shed from animal skin or hair)
- Clothing: certain materials, particularly synthetic fibers, wool, and rough materials can irritate the skin and trigger an allergic reaction
- Sweating: prolonged dampness of the feet from sweating can trigger foot eczema. This is more likely if you are wearing tight shoes, wool socks, or wear socks in bed
- Friction: rubbing over the skin from tight shoes or socks can irritate the skin, particularly if there is already some mild foot eczema – the skin around the foot becomes extra sensitive
- Illness: Dermatitis often flares up when you have a cold or upper respiratory tract infection
How Do You Cure Foot Eczema?
Whatever type of foot eczema you have, the treatment will be basically the same, the aim being to reduce the itching and inflammation during a flare-up and to encourage skin moisture in between.
There is no cure for dermatitis but there are a number of things you can do to manage it by relieving the symptoms and reducing the chance of flare-ups. Early treatment is vital to prevent symptoms from escalating so it is important not to ignore the warning signs of dry, itchy skin.
Treatment is important both during and between flare-ups of foot eczema to help both treat and prevent the condition.
1. Emmolients
Keeping the skin well moisturized is very important with foot eczema. Emollients are medical moisturizers that help to reduce moisture loss from the skin by evaporation and repair its natural protective barrier.
Emollients should be used for treatment and prevention both during flare-ups and during symptom-free periods.
Generous amounts of emollient should be applied at least twice a day when you are symptom-free and more often during flare-ups.
Avoid rubbing emollients into the skin, instead gently apply them following the direction of the hairs to prevent any clogging.
There is a whole range of emollients out there and you may need to try a few before you find the right one for you.
2. Corticosteroids
Corticosteroid creams and ointments can help to reduce inflammation. Over-the-counter medication such as 1% hydrocortisone may be sufficient but in more severe cases your doctor may prescribe stronger corticosteroids. Corticosteroids work best when they are applied around half an hour after moisturizing.
In my experience, ointments tend to be more effective than creams as they contain more oil, soak in better, and are absorbed over a longer period making them more effective at keeping moisture in, but they are greasy. You should continue to use corticosteroids for two days after a flare-up has settled to ensure any inflammation under the skin is fully treated. Eczema On Feet.
Using strong corticosteroids for long periods can lead to skin thinning and/or lightening, acne, and increased hair growth. These side effects usually settle once treatment is stopped.
3. Antibiotics
If the skin has become infected your doctor may prescribe antibiotics to treat the bacteria causing the infection. They may be oral antibiotics or antibiotic creams depending on the infection.
4. Anti-Histamines
Anti-histamines help to reduce itching from eczema by blocking the effect of histamines in the blood.
There are two types of anti-histamines are available:
Sedating Anti-histamines: such as diphenhydramine (Benadryl) cause drowsiness and can be helpful if your foot eczema is affecting your sleep.
Non-sedating Anti-histamines: such as cetirizine (Zyrtec) do not make you drowsy so can be used during the day
5. Bathing
Regular baths and showers can help to reduce the symptoms of eczema but if not done correctly they can make things worse. Bathing (or showering) for 10-15 minutes in lukewarm water helps the skin to absorb moisture and is also a good way to de-stress. Eczema On Feet.
The mantra to follow is “Soak and Seal”. Make sure that you limit soaking to under 15 minutes and that the water is lukewarm, not hot. Avoid scrubbing your skin or using any soaps or solutions that could irritate your skin.
Once out of the bath, gently pat dry your skin with a towel leaving it slightly wet. Then generously apply moisturizer all over the body. This should be done within three minutes of getting out of the bath otherwise the skin will actually become drier and more irritated which is likely to make your foot eczema worse. Allow the moisturizer to soak in for a few minutes before dressing.
It doesn’t matter whether you have a bath or shower with dermatitis, as long as you follow the Soak and Seal method. Products that can help include:
- Bath Oil: to help lock in moisture
- Baking Soda: helps to reduce itching
- Mild Bleach Solution: this can help to decrease inflammation. Use half a cup of household bleach for a full tub. Always rinse off the water before getting out of the bath
- Oatmeal: Colloidal oatmeal such as Aveeno can help to reduce itching
- Vinegar: Can be added to the bath to kill bacteria. Use between one cup and one pint per full tub
Always use products that are free of perfumes and dyes to prevent any irritation when washing.
6. Bandages & Wet Wraps
Wearing special medicated bandages, and socks or placing wet wraps over the affected areas of skin can help to stop the area from drying out, protect the skin, allow it to heal, and prevent scratching.
Emollients and/or corticosteroids should be applied first. This can be particularly helpful if your foot eczema bothers you at night as it helps the cream/ointment to be absorbed and stops you from scratching. Eczema On Feet.
7. Phototherapy
Severe cases of eczema can be treated with UV (ultraviolet) light which helps to reduce inflammation and itching and increases vitamin D production.
Self-Help For Foot Eczema
There are some lifestyle changes you can make to help to reduce the frequency and intensity of foot eczema flare-ups.

- Soak Your Feet: If you don’t want to have a bath/shower every day, soaking your feet daily can help to reduce the itchiness and inflammation of foot eczema.
-
- Make sure you still follow the soak and seal technique described above
- Avoid Scratching: try not to scratch or rub areas of foot eczema as that can further damage the skin and increase the risk of infection.
-
- Keeping your nails short, covering eczema in bandages, or wearing gloves can help with this
- Stress-Management: Learn to recognize and manage stressful environments. Therapies such as CBT (cognitive behavioral therapy) can really help as can relaxation techniques
- Identify Allergens: Try to identify any products that trigger your eczema. For example, try changing washing powder or soap, and keep a food diary
- Keep Your Feet Dry: Foot eczema is made worse by sweating so make sure you regularly let your feet breathe. Go barefoot whenever possible and when you do need to wear shoes, wear 100% cotton socks. Alternate shoes each day to make sure they have dried out fully
What Else Can Help?
Dermatitis is just one of the possible causes of foot rashes and foot lumps. Other conditions such as athlete’s foot and psoriasis can cause dry skin and itching which may mimic eczema.
Remember, managing eczema is a daily thing. It is really important to regularly moisturize even when you are symptom-free to stop your foot eczema from flaring up again. Eczema On Feet.
The article was originally published here.


Comments are closed.